A TB worker, Kyrgyzstan
Yulia Aleshkina works as a Monitoring & Evaluation Specialist (M&E) for the UNDP / Global Fund project. In this blog she shares results of a survey conducted in May 2020 among health care workers to know how they were adapting their work during the Covid-19 pandemic, and what lessons we can take from it.
Health care workers are the main warriors on the front line of the fight with Covid-19. Our project, financed by the Global Fund to fight AIDS, Tuberculosis and Malaria, works with medical workers who care for people living with HIV (PLHIV), people who inject drugs (PWID) and patients with tuberculosis (TB).
When the first Covid-19 cases were diagnosed in our country and when the emergency state was declared, while we were all staying safely at home, medical workers had to carry a new burden on their shoulders: in addition to their usual tasks, which had to be continued in new conditions, they had to start undertaking completely new and difficult responsibilities.
In order to know what problems medical workers faced to deliver services to our project’s clients during the pandemic, the UNDP conducted an online survey from 10 to 15 May among medical personnel from organizations working with PLHIV, PWID and TB patients. We sent the link to the survey to specialized medical organizations (AIDS Centers, Regional TB Centers, the Republican Narcology Center). Honestly, we hadn’t expected such a large turnout: 753 health care workers from all care levels participated in this survey. This response suggests that they have something to say and that they want to be heard.
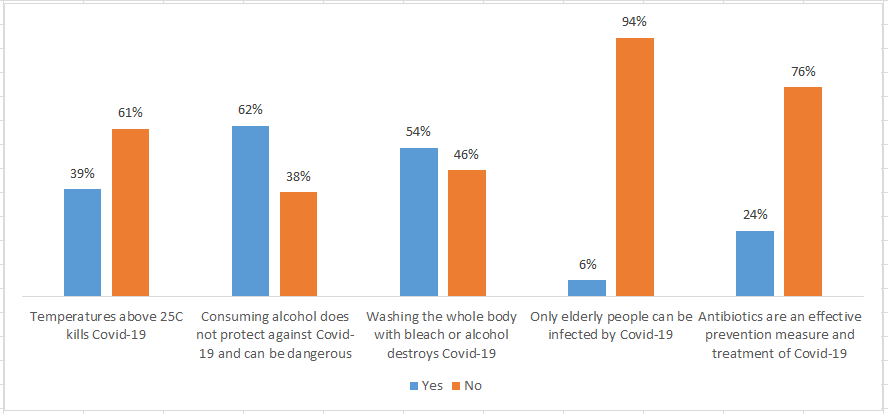
A third of medical workers have distorted knowledge on Covid-19
The first bloc of questions in our survey was linked with medical workers’ knowledge on Covid-19. The survey was conducted two months after the appearance of the first Covid-19 cases in Kyrgyzstan, and, according to official information, all health care workers were trained on the new virus. However, the survey showed that one in three health care workers had distorted knowledge on Covid-19 and prevention measures. For example, 39% of the respondents said that coronavirus dies upon temperatures above 25C, and 54% said that washing your body with alcohol or bleach destroys the virus – which are both false statements.
A third of the respondents (32%) said that even at the end of April / beginning of May, they continued to feel a lack of knowledge on Covid-19 and on how to continue working with PLHIV, TB patients and PWID in these new conditions.
Medical workers are a key expert source of information for the society. For instance, believing that the virus dies when the temperature is above 25C can not only negatively influence the doctors’ own personal hygiene and safety measures, but also change the recommendations which they give to the population, for example on the need to wear a mask in public transport and shops during summer, when the temperature is usually above 30C.
Therefore it is very important to continue providing correct information to health care workers on a regular basis during the pandemic. The new country proposal to the Global Fund on Covid-19 response includes a series of trainings for medical workers and NGO personnel working with PLHIV, TB patients and PWID. But until the implementation of this new grant, the question of education of medical workers remains unanswered.
85% consider that preventive measures within their institutions are effective.
Health care workers’ sense of protection and belief that the risk of Covid-19 infection at work is minimal directly affect their motivation and readiness to fulfill their responsibilities, as well as their relationship to patients.
Medical workers’ opinion on the infection risk at work was split: 41% said that the risk was high (mainly medical staff working in primary health care organizations), 26% said it was low, and the rest evaluated the risk as medium. But 85% of the respondents consider that preventive measures against Covid-19 taken by their organizations were effective. However, if we look at the answers in detail, we see that these preventive measures are clearly insufficient:
- Only 66% of respondents said they were given personal protection equipment (PPE); this means that almost a third of them did not have PPE at the moment of the survey.
- Express screening for Covid-19 symptoms wasn’t conducted in all organizations; only two thirds of respondents said this measure was being carried out. The lack of primary screening and triage of patients can lead to devastating consequences, as show the Covid-19 outbreaks in the National Oncology Center, National Hospital, maternity hospitals and others.
- Only 63% said that they had received clear instructions on how to carry out their work in the new conditions.
- The strategy of decreasing patient visits in the medical centers was mostly undertaken in the AIDS Centers and Family Medical Centers.
- 13% of respondents said that there were cases when patients with Covid-19 symptoms were refused services, which is alarming.
When analyzing these answers, we were concerned by the fact that even mid-May there wasn’t a unique strategy for staff safety among these organizations. None of the above measures were named by a majority of respondents.
Most of the health care workers link their risk of contamination not with the fulfillment of their usual duties (figure 2), but with other factors: visiting public places and performing additional work.
On the one hand, it’s a good news that only 34% of respondents fear that key population groups can become a source of infection, because this can lower the level of additional stigma against people with TB or HIV and clients of the methadone therapy program. But on the other hand, underestimating the risk can lead to tragic consequences: there are already cases when doctors were infected by patients who did not have Covid-19 symptoms or said that they had not been in contact with a Covid-19 patient.
The workload has increased several times.
We also learned through this survey what medical organizations were doing so that patients with HIV and TB and clients of the methadone therapy program could continue taking their treatment in the new conditions imposed by the pandemic, including limited movement.
The results showed that since the detection of the first Covid-19 cases, health care workers’ workload had increased several times. According to the respondents, demands for diagnostic, consultation and treatment for TB and HIV decreased, but their workload was increased due to other unusual responsibilities. 58% of medical staff was directly involved in activities related to Covid-19: at-home-visits, disinfection, caring for patients in quarantine centers, investigating contacts…
In order to guarantee continued access to medical services for patients and clients, the following measures were taken (figure 3): phone consultations, at-home-visits, distribution of PPE, implementation of video observed treatment, delivery of medication at home. People living with HIV were given their treatment in advance for a period of up to three months, while patients with TB were given medication for 14 days, and clients on methadone for up to 1 week.
Given the current situation and experts’ prognosis, the practice of distant medical services will be implemented on a large scale. Results of the survey confirmed that political will alone is not sufficient to implement new methods. Organizations that had already introduced alternative treatment methods were able to rapidly adapt to the new reality and provide uninterrupted access to medication, whereas it was more difficult for organizations that had never faced such a need before. Even within specific institutions, there is an absence of a common strategy to provide quality services to patients: methods are being developed separately by each department and depend on the political will of the direction, the professionalism of the personnel and the organization’s resources.
Therefore, the UNDP / Global Fund project continues to provide technical and consultative support to medical organizations regarding uninterrupted access to medical services: we monitor alternative treatment methods, develop instructions, and plan to hire additional consultants in this regard. In the framework of the new Global Fund grant, additional resources were requested to organize mobile brigades, hire case managers and extend access to video observed treatment.
Health care workers remain our main resource in the fight against the new pandemic, and, unfortunately, among the most vulnerable group to the new disease. In the first weeks of the pandemic in Kyrgyzstan, the rate of medical workers among people infected with Covid-19 was 20-24%, on July 6th it was 15-18% (1147 out of 7691). At the same time we have to admit that we are still only at the beginning of our fight against Covid-19.
What did this survey show? First of all, I want to highlight that in the past few days health care workers were faced with yet again new conditions and had to react to the outburst of the pandemic. They were able to adapt their services and to accept additional workload. They continue to help their patients in the limit of their possibilities and efforts, regardless of the difficult situation and limited resources.
We also see that despite the time that was given to prepare during quarantine, there are still a lot of unanswered questions. There is a long path ahead of us, and we are just coming to the first peak of the pandemic. Health care workers shouldn’t be alone in this fight. We – the government, non-governmental organizations, donors, projects, businesses, and society as a whole – have to do everything we can to lessen their workload, help them continue working and protect them from infection.

 Locations
Locations